With March being Deep Vein Thrombosis (DVT) Awareness Month, we want to dedicate this blog post to the causes of DVT and its dangers.
According to the American Heart Association, up to 2 million Americans are affected by DVT each year, and, according to a recent national survey, 74% of them have little or no awareness of the condition. This makes it especially important to know what to look for.
Deep Vein Thrombosis Warning Signs
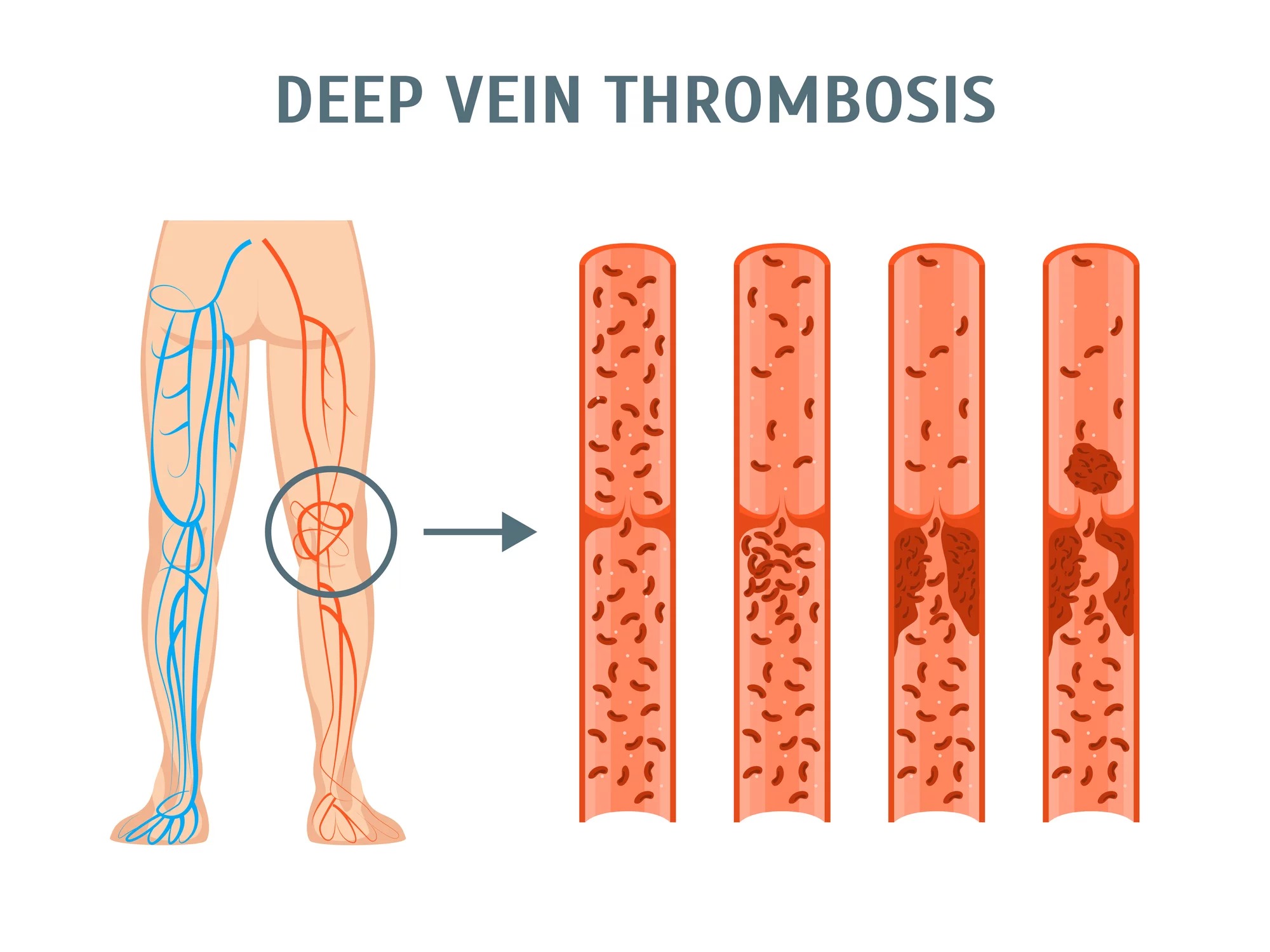
DVT is a dangerous condition that occurs when a large vein, deep in the leg or pelvis, develops a blockage or clot. This condition must be addressed as, if left untreated, it can cause major health problems. The most serious risk of a DVT is that of a pulmonary embolism. That occurs when a piece of the clot breaks off from the leg and travels through the bloodstream to the lung. This affects the ability of the body to get oxygen and, in some situations, may lead to death.
Learn about the 7 Misconceptions of Varicose Vein Treatment
Unfortunately, many times DVT is without symptoms until a pulmonary embolus occurs! Often a DVT can produce leg swelling, soreness when you walk or stand, or a heavy feeling in a leg that is not typical of your normal condition. Here at the Vein Institute of NJ, our vascular surgeons are highly trained with significant experience diagnosing and treating this condition.
What Causes DVT?
There are risk factors for DVT that are important to recognize, some more common than others. Below are a few of the lesser known risks, which may surprise you and should be heeded:
- Long periods of travel can put you more at risk due to prolonged sitting and, on airplanes, changes in cabin pressure with altitude. It is helpful to contract your calf muscles—ankle rolls are great exercises—every 30-60 minutes if possible.
- Estrogen-based medicines such as birth control and hormone replacement therapy can, in some people, increase the risk of DVT. Be sure to discuss these with your physician—particularly if there is a family history of blood clotting.
- Cancers have been linked to high rates of DVT along with some types of chemotherapy. It’s important to remain active and wear compression hosiery during treatment as much as possible.
- Studies have shown that those with Inflammatory bowel disease (IBS, Crohn’s disease, ulcerative colitis) can have an increased risk of developing blood clots.
- Pregnancy has been known to cause blood clots with many women still at risk for up to 6 weeks after they give birth. Being active can help reduce those risks.
What Types of Treatment are Available for Deep Vein Thrombosis?
There are several options available to treat DVT. We recommend consulting with an experienced, board-certified vascular surgeon to understand all of your particular options.
- Blood thinners. DVT is most commonly treated with anticoagulants, also called blood thinners. They don't break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots or having the clot you have travel.
- Clot busters. If you have a more serious type of DVT or pulmonary embolism, or if other medications aren't working, your doctor might prescribe drugs that break up clots quickly, called clot busters or thrombolytics.
- Filters. If you can't take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs.
If you are experiencing any signs of DVT or would like to learn more about risk factors and prevention, schedule an appointment with one of our vein treatment specialists who can discuss your situation with the knowledge to determine your best course of action.




_2.jpg)