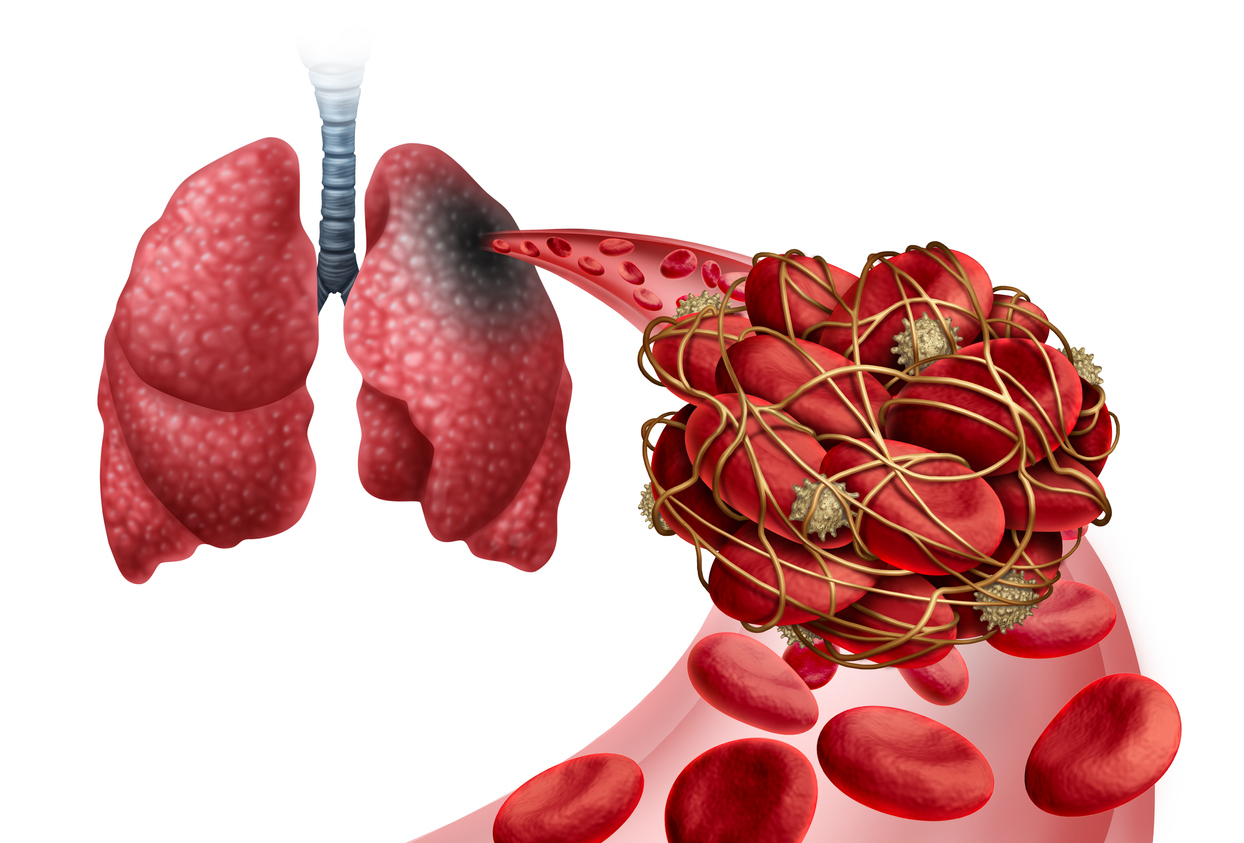
Inferior Vena Cava (IVC) filters are medical devices that play a crucial role in preventing life-threatening complications in certain patients. These filters are designed to capture blood clots that may break loose from deep veins in the body and travel to the lungs, causing a pulmonary embolism.
In this blog, we will delve into what IVC filters are, why they are used, how they are inserted, and what patients can expect during and after the procedure.
What is an IVC Filter?
The inferior vena cava (IVC) is the largest vein in the body, responsible for returning deoxygenated blood from the lower half of the body to the heart. IVC filters are small, spider-like devices made of metal or synthetic materials. They are designed to be inserted into the IVC to prevent blood clots from reaching the lungs, where they could lead to a pulmonary embolism.
Why IVC Filters Are Used
IVC filters are used in specific medical situations when there is a risk of blood clots traveling to the lungs. Some common reasons for using IVC filters may include:
- Deep Vein Thrombosis (DVT): IVC filters are often recommended for individuals with a history of DVT, a condition characterized by the formation of blood clots in deep veins, typically in the legs.
- Pulmonary Embolism Risk: Patients who are at a high risk of developing pulmonary embolisms due to factors such as surgery, trauma, or immobility may receive IVC filters as a preventative measure.
- Contraindications to Anticoagulants: In cases where patients cannot use anticoagulant medications due to a bleeding disorder or other medical condition, IVC filters can provide an alternative means of preventing pulmonary embolisms.
How IVC Filters Are Inserted
The insertion of an IVC filter is typically performed by a vascular surgeon or interventional radiologist and usually takes place in a sterile operating room or interventional radiology suite. Here's a brief overview of the insertion procedure:
- Preparation: The patient will receive local anesthesia to numb the area where the filter will be inserted, usually in the groin or neck.
- Guided Insertion: Using real-time imaging guidance, the physician will insert a catheter (a thin, flexible tube) through a small incision into a vein in the designated area. This catheter is then advanced to the IVC.
- Placement: The IVC filter is carefully threaded through the catheter and positioned in the desired location within the IVC. Once in place, the filter's legs or struts open, anchoring it securely.
- Catheter Removal: The catheter is withdrawn, and the incision is typically closed with a small suture or adhesive.
- Recovery: After the procedure, the patient is monitored for a short period to ensure there are no immediate complications. In many cases, patients can return home the same day or after a brief observation period.
What You Can Expect After the Procedure
- Recovery: Recovery time after an IVC filter placement is usually minimal. Patients may experience some soreness or bruising at the insertion site, but this discomfort typically resolves within a few days.
- Post-Procedure Care: Patients will receive specific instructions on how to care for the insertion site, including keeping it clean and dry. Any unusual symptoms or signs of infection should be reported promptly to the healthcare provider.
- Regular Follow-up: Patients with IVC filters will need regular follow-up appointments with their healthcare provider to monitor the filter's effectiveness and assess any potential complications. Depending on the patient's condition, the filter may be removed or left in place permanently.
- Potential Risks: Like any medical procedure, IVC filter placement carries some risks, including infection, bleeding, filter migration, or device-related complications. It's essential for patients to be aware of these risks and discuss them with their healthcare team.
IVC filters are important medical devices that can save lives by preventing pulmonary embolisms in high-risk patients. While IVC filters are highly beneficial in certain situations, the decision to use them should be made in consultation with a medical professional who can assess the patient's individual risk factors and medical history.





_2.jpg)